Background: Purpura fulminans (PF) is a rare but devastating complication of sepsis in which patients experience overwhelming systemic thrombosis leading to end organ damage, distal limb ischemia, and death. Survivors are often left with lifelong disfigurement and/or disability due to severe acral tissue injury and the need for amputation of necrotic extremities. Given that most patients who develop PF have no known underlying medical conditions and are much younger than those typically afflicted with sepsis, we sought to investigate whether genetic determinants predispose individuals to developing PF.
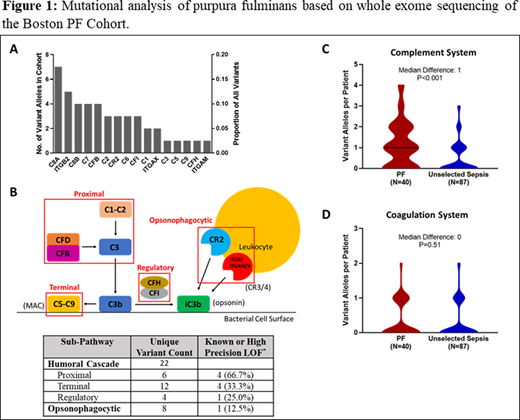
Methods: We performed whole exome sequencing on the Boston PF Cohort (N=40). We used pathway-based collapsing analysis (PBCA) combined with mutational burden testing to evaluate for enrichment of rare coding variants in the complement system using as a comparator unselected patients with sepsis from the NHLBI ARDSnet iSPAAR cohort (N=87). Several novel variants in integrin complement receptors were identified and subsequently cloned and functionally characterized.
Results: Patients in the Boston PF Cohort were relatively young at the time of presentation, with a median (IQR) age of 37.5 (20.3-58.8) years. Patients were afflicted with gram negative organisms 45% of the time, while 27.5% were infected with gram positive organisms. In another 27.5%, no pathogen was identified. PF patients had strikingly abnormal markers of severe sepsis and coagulopathy, including the following median (IQR) values: lactate 7.1 (5.3-11.8) mmol/L, platelet count 28,000 (15,000-48,500) per μl, aPTT 68.0 (48.3-142.5) seconds, INR 2.8 (1.9-4.0), and protein C activity 26.0% (13.5-38.5). No patient had a known congenital immune defect. Whole exome sequencing (mean read depth 80X) identified 30 unique heterozygous complement system variants in 26/40 (65%) patients with PF (Figure 1A-B). Variants in this pathway were highly enriched in PF patients compared to the control cohort (P<0.001, Figure 1C), and the signal remained significant (P=0.02) in a sensitivity analysis comparing only Caucasian patients. By contrast, no enrichment of variants was found in the coagulation system (P=0.51, Figure 1D), and no difference in complement system variants was detected between the two cohorts when only synonymous variants were considered. The number of complement system variants per patient correlated positively with their Sequential Organ Failure Assessment (SOFA) score at the time of presentation (P=0.03) and independently predicted presenting SOFA score in a multivariate regression model (P=0.04). Eleven unique variants were identified in ITGAM, ITGAX, and ITGB2, genes encoding the integrin complement receptors 3 and 4 (CR3 and CR4), which have anti- and pro-inflammatory properties, respectively. Because little is known about the function of these receptors in sepsis, we performed additional in vitro studies and found that 6/8 (75%) CR3 variants resulted in partial or complete loss-of-function, while 3/7 (42.9%) CR4 variants unexpectedly resulted in gain-of-function. Taken together, these results suggest that the immune response to microbial infection in PF patients results in enhanced pro-inflammatory signaling by CR3 and CR4.
Conclusions: Our data suggest that rare inherited defects in the complement system predispose individuals to the maladaptive thrombo-inflammatory response to infection that characterizes PF. By advancing our understanding of the molecular pathogenesis of PF, this work could provide important insights into the broader problem of coagulopathy in sepsis. Furthermore, targeted gene discovery approaches based on PBCA may serve as a model for future genomic studies of rare hemostatic diseases.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal